Thoracic Outlet Syndrome
What is thoracic outlet syndrome?
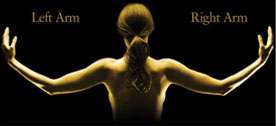
The nerve roots that exit the various levels of the spinal cord merge to form the brachial plexus which gives rise to the various peripheral nerves of the upper extremity. The brachial plexus merges superior to the clavicle or collar bone through a triangle composed of the anterior scalene muscle medially, the middle scalene muscle laterally, and the first thoracic rib at the base of the triangle. It is within this tight space that the brachial plexus is subjected to injury or compression.
What causes thoracic outlet syndrome?
- Cervical ribs (normally there are only thoracic ribs).
- Congenital fibrous bands.
- Tumor.
- Anomalous muscle insertion or origin.
- Muscle spasm secondary to cervical spine abnormality.
- Vascular abnormality such as a subclavian artery aneurysm.
What are the symptoms of thoracic outlet syndrome?
- Numbness and tingling of the entire upper extremity or hand.
- Paresthesias (tingling) of the arm and hand (more common in the little, ring, and middle fingers).
- Nocturnal symptoms of pain and paresthesias.
- The hallmark of this diagnosis is reproduction of symptoms with use of the limb in an elevated position such as combing the hair.
- Exacerbation of symptoms with the arm in a forward reaching position such as when carrying things or driving.
- Pain in the supraclavicular area (above the collar bone), shoulder, neck, and occasionally headaches.
- If vascular abnormality is present, there may be cyanosis with activity of the upper extremity if arterial in origin. Swelling of the extremity occurs if venous in origin.
How to diagnose thoracic outlet syndrome
In addition to a careful history of the symptoms described above, an examination will reveal:
- Tenderness and swelling at the supraclavicular fossa (above the collar bone).
- Provocative tests (Wright maneuver): Reproduction of symptoms with abduction and external rotation of the shoulder.
- Sensibility is usually normal.
- Muscle weakness or atrophy (unusual).
Additional tests may be helpful:
Lordotic chest x-ray:
to evaluate the apices of the lungs where tumors can arise that can cause symptoms of thoracic outlet syndrome.
Cervical spine series:
To evaluate the integrity of the cervical spine as well as to assess if there are any cervical ribs present.
MRI:
To assess the cervical spine nerve roots for possible points of compression.
CT scan:
Performed occasionally if there is a history of trauma to evaluate the first thoracic rib for possible fractures.
Electrodiagnostic tests:
Rarely helpful in revealing thoracic outlet syndrome. However, can be helpful in looking at other causes in the differential diagnosis such as peripheral nerve entrapment.
Non-surgical treatment for thoracic outlet syndrome
Physical therapy with postural reeducation, levator scapulae, and trapezius muscle strengthening; weight loss is advised in obese patients; proper breast support is indicated for patients with large breasts and occasionally even reduction mammoplasty; work modification limiting overhead work of the arm; NSAID’s (i.e. Advil) or steroids; if the patient’s symptoms continue after four months of conservative therapy to an unacceptable level, then surgery is indicated. Obviously, impending vascular compromise is an immediate indication for surgery.
Surgical treatment of thoracic outlet syndrome
Supraclavicular approach with division of the anterior and middle scalene muscle insertion and removal of the first thoracic rib. There is approximately a 20% chance that this surgery will not be successful mainly because the diagnosis is purely clinical and there is approximately a 20% chance of an inaccurate diagnosis. There is approximately a 20% chance of a pneumothorax which is quickly resolved following a drain placement overnight. Symptoms should resolve quickly, if not immediately, following surgery. There is a small risk of phrenic nerve injury with paralysis of the diaphragm on the operative side and a very small risk of vascular or nerve damage from the surgery.
Patient is kept in the hospital for two days with a drain placement during this time to prevent hematoma collection. The patient is also kept in the hospital for pain control during this 48 hour period. The patient then goes home to activity as tolerated. Unless weakness was present preoperatively, therapy is usually not necessary following surgery.
How can Dr. Knight help you with thoracic outlet syndrome?
Dr. Knight has an extensive knowledge of nerve problems throughout the upper extremity to the neck. Frequently, patients have had multiple surgeries without relief of symptoms with this condition. Dr. Knight will rule out all common causes of arm pain and numbness to narrow in on this diagnosis. Once he confirms the diagnosis of thoracic out left syndrome, he will take you through an exhaustive program of conservative treatment leaving surgery as a remote last resort.
Disclaimer
HandAndWristInstitute.com does not offer medical advice. The information presented here is offered for informational purposes only. Read Disclaimer